The problem:
It’s not uncommon for people with recurrent episodes of back pain to become fearful and to start avoiding activities in life. They begin to associate pain with the activity and that the activity is doing harm. Thus, in their minds, pain equals harm and any activity that causes pain avoided. The problem becomes that as this the list of activities grow, deconditioning sets in and begins to feed into back pain. At this point, most figure they are just “getting old” or figure they will need to “learn to live with the pain”. The reality is there is a solution to help you fight against these feeling of fear and limitation and enable you to fight dysfunction in your body.
The solution:
Research tells us that exercise should be part of your back pain solution. This isn’t true of just backs, as exercise should be part of any joint pain solution. Time and time again, more than any other intervention, exercise has demonstrated the ability to provide positive outcomes in back pain relief and reduced relapses. However, too often people use different exercises to help reduce their pain only to find that exercise makes their back feel worse. The solution isn’t just simply exercise, the solution is understanding the right exercises to do while also understanding which exercises to avoid. You need to know what exercises for sciatica and disc herniation are best to do 1st to create a good foundation of movement before progressing to more difficult exercises. Where do you go for that information? Over the past several years we have put together a clinically successful exercise progression program for our patients and clients with back pain. These exercise progressions serve as the framework for rehabilitation and also serve as the foundation for improving athletic performance. Join us for our Core Training – From Rehab to Performance workshop and learn more about what you can begin doing immediately to help reduce your back pain, feel better, and improve your performance in sport or life.
More related reading:
https://gallagherperformance.com/the-best-exercise/
WHAT ARE MY OPTIONS IF YOU DON’T TAKE MY INSURANCE?
The insurance industry has become increasingly difficult to work with as many large carriers have limited or completely closed off providers from joining their network.
In such cases, we operate as a fee-for-service facility and offer affordable plans that truly increase the value of our patient’s experience. But rather than take my word for it, let's do the comparison between traditional chiropractic and the difference at Gallagher Performance.
TRADITIONAL CHIROPRACTIC
Most traditional chiropractors spend 5-15 minutes per patient and often attempt to have them come 2-3 times per week for an extended period of time. Most patients only experience passive modalities and adjustments with a predictable routine of stim-heat-adjust-out the door. And if there is rehab, often it is supervised by unlicensed aides who instruct patients in exercises. Most traditional chiropractors will see a patient 18-24 times in order to resolve their problem. Depending on co-pay or co-insurance, the out-of-pocket expense can add up quickly. For someone who has a $25 copay, that means they will have $450-$600 of out-of-pocket expense.
THE GALLAGHER PERFORMANCE DIFFERENCE
At Gallagher Performance, you spend 30-60 minutes with your chiropractor, enabling faster recovery in fewer visits. Most of our patients recover in less than 8 visits, spend 100% of their time 1-on-1 with a board-certified rehabilitation chiropractor, and are provided with essential knowledge and tools needed to ensure pain doesn’t come back. Our approach will actually save you money while providing you with a higher quality of treatment. That’s value you can’t compare!
Gallagher Performance Receives 2016 Best of Pittsburgh Award
Pittsburgh Award Program Honors the Achievement
Gallagher Performance has been selected for the 2016 Best of Pittsburgh Award in the Chiropractors category by the Pittsburgh Award Program and is among a very small group of businesses that have won the Best of Pittsburgh Award for three consecutive years.
Each year, the Pittsburgh Award Program identifies companies that we believe have achieved exceptional marketing success in their local community and business category. These are local companies that enhance the positive image of small business through service to their customers and our community. These exceptional companies help make the Pittsburgh area a great place to live, work and play.
Various sources of information were gathered and analyzed to choose the winners in each category. The 2016 Pittsburgh Award Program focuses on quality, not quantity. Winners are determined based on the information gathered both internally by the Pittsburgh Award Program and data provided by third parties.
About Pittsburgh Award Program
The Pittsburgh Award Program is an annual awards program honoring the achievements and accomplishments of local businesses throughout the Pittsburgh area. Recognition is given to those companies that have shown the ability to use their best practices and implemented programs to generate competitive advantages and long-term value.
The Pittsburgh Award Program was established to recognize the best of local businesses in our community. Our organization works exclusively with local business owners, trade groups, professional associations and other business advertising and marketing groups. Our mission is to recognize the small business community's contributions to the U.S. economy.
SOURCE: Pittsburgh Award Program
How Movement Improves Brain Function
Movement is essential to the function of our heart, lungs, and lymphatic system. Movement is critical to keeping our muscles, joints, cartilage, and connective tissue healthy. Movement aids in the delivery of oxygen and nutrients throughout our body and assists in removal of metabolic waste products.
These are points that the majority of us have either heard about or have come to understand about the importance of movement as it relates to our overall health.
Yet one major benefit of movement is often overlooked - the stimulation of pathways required for proper brain and body function.
Yep, that’s correct. Movement - especially of the spine - is required for proper brain function and coordination of activities such as concentration and learning, motor control, emotions, and optimizes organ and immune function.
There is a reason why you experience an increase in mental alertness after exercise or even a visit to the chiropractor. According to Roger Sperry, Nobel Prize recipient in Brain Research, movement of the spine generates 90% of the nerve stimulation used to run the brain.
The brain does not simply control the body, the brain requires constant stimulation and that stimulation comes from movement.
Movement charges your brain’s battery and enables you to think, function, and feel better.
Sound a bit too good to be true?
The work of some of the most prominent neurologists and physiologists in the world continually support the role of movement in brain and nervous system health.
The stimulation your brain receives from movement – once again, especially of your spine – is now being considered essential to optimal brain function and development. In fact, research is now showing that people who do not adequately stimulate their brain through movement have learning, memory, emotional, and behavioral deficits.
This is especially true for children because spinal joint receptor stimulation plays an integral role in the development of the child’s brain and nervous system. The effects of decreased stimulation of the brain in childhood have been linked to central motor impairment, developmental impairments, learning disabilities, and concentration problems like ADHD.
Regardless of your age, the message should be clear at this point: Movement does a body – and brain – good.
Get out and get moving.
More related reading:
https://gallagherperformance.com/tips-on-recovery-and-restoration/
https://gallagherperformance.com/does-practice-make-permanent-how-practice-rewires-your-nervous-system/
A Solution to Headaches
Headaches are among the most frustrating and debilitating conditions seen by healthcare practitioners, from primary care physicians to chiropractors. When severe enough, headaches may interfere or prevent even the most basic daily activities that we take for granted, such as thinking, talking, and reading.
While a logical assumption would be that the origin of headaches is in the head itself, science suggests many of the most common headaches are generated from the joints, muscles, and nerves of the neck.
The head and neck is an inherently unstable system that requires a complex neuromuscular system to surround the spinal column for control of movement and protection from injury.
Many daily activities, such as prolonged sitting and poor posture, can affect the function and health of the joints, muscles, and nerves of the neck. Poor posture or prolonged postures common to students and the majority of the working class can lead to muscular imbalances, restricted joint motion, and unnecessary strain on the neck and upper back often responsible for headaches.
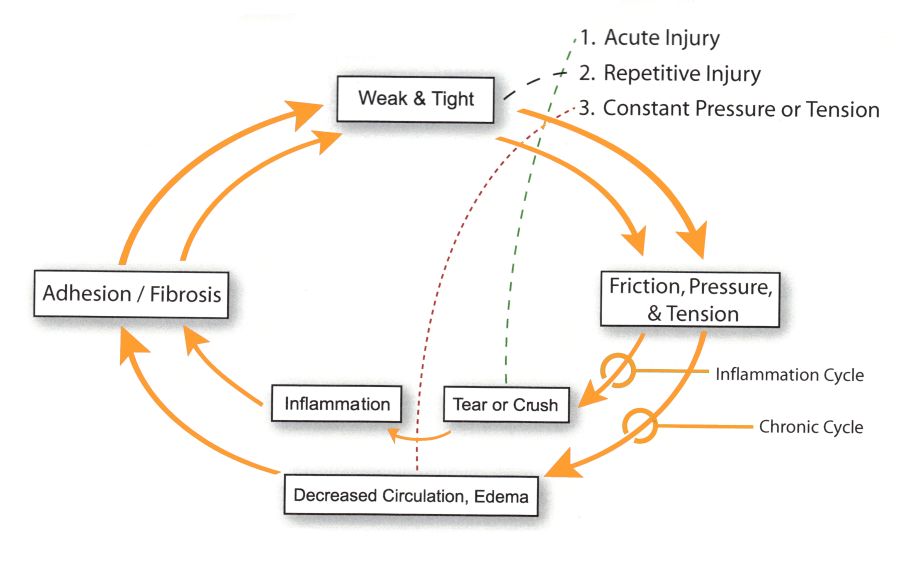
Referred pain and micro-trauma explain how this strain often results in headaches. Referred pain is a neurological phenomenon which is responsible for the perception of pain at a location other than where the problem exists. Using the headache as our example, the problem exists in your neck or upper back, yet your symptoms and perception of pain exists in your head. Micro-trauma is cumulative, small scale damage that occurs in and between soft tissues (muscles, tendons, joint capsules, ligaments and nerves) in response to strain. The bodies response to this strain is to lay down small amounts of repair tissue. Over time, a build up of repair tissue can form adhesions or scar within the soft tissue altering function. Left untreated, these adhesions often lead to pain, tightness, stiffness, restricted motion, and diminished blood flow. The result is a negative feedback cycle, the cumulative injury cycle.
So how do we stop the cycle?
Massage therapy, myofascial release, and IASTM (instrument assisted soft tissue mobilization) techniques are just some of the tools utilized at Gallagher Performance to address scar tissue adhesions and neurological dysfunction in soft tissue. Along with these tools, we often utilize chiropractic manipulative therapy (adjustments), sensory motor stimulation, and Dynamic Neuromuscular Stabilization (DNS) to improve posture, positional awareness, and help restore muscular balance. The combination of these therapies have helped numerous patients find a solution to chronic headaches or migraines.
The next time your dealing with a headache, consider Gallagher Performance. There is a solution to headaches that doesn't involve taking medication. Call our office at (724) 519-2833 to schedule your appointment.
More related reading:
https://gallagherperformance.com/fascia_muscular-adhesions_how_they_relate-_to_pain_and_overuse_injuries/
https://gallagherperformance.com/powerful-innovative-approach-improving-body-functions/
https://gallagherperformance.com/why-stretching-wont-solve-your-tight-muscles/
4 Reasons Athletes Get Adjusted
There is a reason why countless professional and Olympic athletes receive regular chiropractic care. The physiologic and neurologic benefit of spinal manipulation is super charged when used in a comprehensive care plan to address pain and dysfunction.
This infographic puts it into words nicely!
The Benefits of Spinal Manipulation
Spinal manipulation, also known as Chiropractic Manipulative Therapy, is an effective and efficient way to improve joint mechanics, reduce pain, improve mobility, and facilitate the acquisition of improved movements patterns when implemented strategically into treatment plans.
Yet the benefits of spinal manipulation, or chiropractic care in general, is still met with skepticism.
We are so far past establishing that there is evidence supporting spinal manipulation. Rather, we are moving in the direction of how to best establish the use of spinal manipulation in the management of specific musculoskeletal conditions and pain syndromes. The fact is that there are so many studies, systematic reviews, and meta-analyses done on spinal manipulation that a Medline search would be overwhelming to discuss.
The evidence is well summed up by a review of international low back pain guidelines. Over the last 10 years, 12 countries have done critical reviews of the scientific literature concerning low back pain. The international consensus is that the evidence supports chiropractic spinal manipulation as an effective tool in managing low back pain, and therefore is included in the recommendations.
However, the benefits of spinal manipulation do not begin and end with back pain. There are numerous benefits to spinal manipulation that make chiropractic care an invaluable addition to one’s health related or athletic pursuits. Below is just a short list.
- Joint pain relief - The most obvious benefit is relief of pain. Chiropractic manipulative therapy (CMT) can almost instantly relieve pain experienced in the low back, mid-back, neck, and extremities and has demonstrated this in research.
- Disc Bulge/Sciatica - The European Spine Journal published the findings from a clinical trial with chiropractic manipulative therapy showing 72% success rate in treating sciatica and associated symptoms. Disc bulges respond favorably to spinal manipulation techniques which focus on resorting joint mechanics and unloading the intervertebral discs.
- Headaches (tension and migraine) – There are hundreds of peer reviewed research articles demonstrating the ability spinal manipulation to prevent and ease the burden of headaches and migraines.
- Blood Pressure - In 2007, a team of researchers published a study in the Human Journal of Hypertension demonstrating that one upper cervical chiropractic adjustment had the same effect as two blood pressure-lowering drugs. Those effects were not simply short-term, they lasted more than six months.
- Surgery Prevention - The Journal of the American Medical Association recently published its low back pain guidelines and suggested that people suffering from back pain first try chiropractic before resorting to surgery. When appropriate, a growing number of physicians and specialists are recommending patients pursue conservative management of musculoskeletal conditions and pain syndromes before surgical intervention. The majority of these patients avoid surgery as they respond extremely well to conservative management via chiropractic care, physical therapy, or a combination.
- Athletic Performance - There is a reason why countless professional and Olympic athletes receive regular chiropractic care. The physiologic and neurologic benefit of spinal manipulation is super charged when used in a comprehensive care plan to address pain and dysfunction. Simply stated, muscles just work better when proper joint motion is restored via manipulative therapy. Athletes thrive on proprioception and motor responses from sensory input. Proprioception and motor response all improve from spinal manipulation. Coupled with exercises to facilitate motor skill acquisition, the short-term responses from spinal manipulation eventually become long-term improvements in movement quality and efficiency.
As stated above, spinal manipulation is a power tool that can be used within a comprehensive treatment plan. These treatment plans often utilize a variety of approaches that emphasize soft tissue work, guided exercises to improve stabilization and movement patterns, and patient education. These combined approaches serve as a “gold standard” for successful management and treatment of a number of musculoskeletal conditions.
To learn more about chiropractic and how it can be a benefit to your health or athletic goals, please contact our office at (724) 519-2833.
More related reading:
https://gallagherperformance.com/solution-long-term-improvement-back-pain/
https://gallagherperformance.com/the-solution-for-chronic-back-pain/
https://gallagherperformance.com/low_back_pain_causes_and_treatment_recommendations/
Low Back Pain Treatments That Just Won't Help
Back pain was believed to be a self limiting condition for the majority of individuals, meaning that the nature of back pain is that it would "run its course" and eventually pain would go away on its own. Current research has demonstrated that this understanding of back pain is flawed; yet many clinicians still hold this belief.
In fact, 85% of people with a single episode of low back pain will likely experience future recurrences and 2-8% of those individuals will develop chronic back pain.
Chronic pain accounts for 75% of all healthcare costs related to low back pain, is second only to the common cold in missed days from work, and is the number one reason for workmen compensation claims.
Considering the burden chronic back pain places on healthcare resources, patient management appears to be an issue in need of addressing appropriately as many patients find it difficult to find effective treatment.
Low Back Treatments That Don't Help
Now many experts are questioning the model in which back pain is treated as a growing body of research suggests many common back pain ‘cures’ just don’t work. These include:
- Ultrasound
- TENS machines
- Strong opium-type painkillers, such as diamorphine
- Spinal injections
- Spinal fusion
- Disc replacement
Top spine expert, Professor Stuart McGill is the world’s leading spinal biomechanics researcher and has identified common reasons for back pain and the importance of exercise as an intervention for effective treatment.
In Dr. McGill's opinion, based on over 30 years of research, every case of back pain has a cause and the reason many treatments are ineffective is because they are used on a one-size fits-all approach, rarely targeting the underlying problem.
There are many possible causes for back pain, but you must first find the positions and stresses that trigger pain. As Dr. McGill says, finding these positions and stressors allows the provider to formulate a precise diagnosis and a roadmap to recovery. This roadmap is guided exercises that can correct the harmful patterns and build a stable, firm spine.
Addressing Misconceptions
The importance of a firm spine can come as a surprise to many, as the common perception is that your back must be flexible in order to be healthy and pain-free.
The spine must be firm and have strong muscles surrounding it to help transmit forces from the legs and the shoulders while minimizing the stress on the spine. When the muscles of the spine aren’t strong enough, micro-movements can occur that eventually can sensitize the spine and lead to a painful back.
If you have some movements, which are comfortable to build on, this opens the door to conservative management and recovery through guided exercise
However, recommendation of exercise without a clear understanding of movement intolerances and muscles that must be strengthened can also be harmful
Guided Exercise: The #1 Intervention for Low Back Pain
Exercise is essential both to protect and repair your back, but simply hitting the gym or doing Pilates or yoga without knowing the movement patterns that are generating your pain or the ones that will protect and build a pain-free back, has little chance of being effective.
Thanks to exercises specifically targeted at a patient’s problems, we are able to help educate them on proper posture and movement so they do not put damaging load on their spine. The guided exercise model is truly about identifying a patient's underlying back pain generators and educating them on not only how they can get out pain, but also what they can do to keep it from returning.
When you consider that 85% of individuals who have low back pain will experience future recurrences, there must be a priority placed on educating patient's about proper posture, movement, and exercises that build a firm, strong spine. Guided exercises are showing clear efficacy for use in patients with low back pain and should be a staple in their treatment plan.
If you are suffering from low back pain, whatever the cause, consider Gallagher Performance for your evaluation and treatment. Our goal is to relieve your pain while teaching you what you can do to keep the pain from returning.
More related reading:
https://gallagherperformance.com/solution-long-term-improvement-back-pain/
VBlog: Overtraining a Myth?
This short video discusses the reality of overtraining as it relates to human performance when it matters most. Overtraining is not a myth. Learn more here.
https://www.youtube.com/watch?v=tyYQEVO7QOI
Dynamic Neuromuscular Stabilization: Advancing Therapy & Performance
Here at Gallagher Performance we not only strive to provide the best in chiropractic, rehabilitation and manual medicine treatments for our patients, but we also utilize comprehensive diagnostic methods and tools to help determine which treatment is best for you. This allows us to apply to most ideal therapeutic interventions. At GP, this could include any combination of the following: chiropractic manipulative therapy, manual therapy according to Lewit and Janda, Vojta Therapy, myofascial release, trigger point therapy, neuromobilizations, and dynamic neuromuscular stabilization (DNS).
Despite many of our patients having previous experience with chiropractic or physical therapy, they are unfamiliar with DNS. Gallagher Performance specializes in DNS therapy. Dr. Gallagher has been studying and utilizing DNS since 2007. His extensive training and background allows him to provide a level of care that is unique to the Pittsburgh area.
Since DNS has implications in both physical rehabilitation and training, we spend a great deal of time educating our patients and clients on DNS and answering some frequency asked questions. With that in mind, the goal of this article is to help educate our readers about DNS and the significance this intervention has as it relates to pain or sports performance.
What is DNS therapy?
DNS is a revolutionary European approach in the treatment of back pain and several neuromuscular conditions. DNS therapy is based on the neuroplasticity of the Central Nervous System and targets the cause of pain/dysfunction rather than its manifestations. DNS therapy evokes ideal movement patterns by manual stimulation of developmental reflex zones and utilizes specific exercises to improve neuromuscular control. The therapeutic benefits become significantly expanded from previous standards of rehabilitation. Any one from infants to adolescents, chronic pain patients to athletes can all benefit from DNS therapy.
How does DNS compliment chiropractic adjustments?
DNS therapy favorably compliments traditional chiropractic adjustments in several ways. When patients may be apprehensive about receiving an aggressive or forceful chiropractic adjustment, DNS offers gentle, non-forceful, low velocity manipulation that is well tolerated and safe. For those that receive traditional chiropractic adjustments, DNS works in concert to normalize joint function and restore muscular balance, leading to more sustainable improvements in reduced pain and improved function.
Often times, symptom relief experienced from a chiropractic adjustment can be short-lived with symptoms returning rather quickly. In contrast, when DNS is applied in a chiropractic setting, the approach allows for longer-lasting symptom relief due to therapy’s ability to improve Central Nervous System (CNS) coordination and joint stability which is then maintained by performing prescribed home exercises.
DNS therapy simply enables a chiropractor to effectively treat and manage a broad range of musculoskeletal and neurological disorders. While traditional chiropractic may be limited in what can be done through chiropractic adjustments and passive modalities, DNS represents a powerful alternative to chiropractic care when dealing with pain syndromes and more complex structural pathologies where the effectiveness of traditional chiropractic is highly limited.
How is DNS therapy able to get me out of pain and moving better when other conservative therapies have failed?
The results achieved by DNS therapy are often difficult to achieve with traditional methods used by chiropractors and physical therapists due to the physiological phenomenon that occurs during treatment to minimize muscular imbalances, relieving painful protective muscle spasms, resulting in a more stable musculoskeletal system with improved spinal stability and postural awareness.
During DNS therapy, induced movements are controlled not locally, but by the higher levels of the Central Nervous System. This then results in faster and longer-lasting improvement in function and pain relief. When combined with exercise, the promotion of joint stability and ideal movement becomes habitual and independent of conscious effort.
How are DNS exercises different from traditional physical therapy or physical training exercises?
In the majority of physical therapy and chiropractic clinics, as well as in personal training settings, exercises are performed that simply train muscles in isolation. The patient who has shoulder pain and is only prescribed shoulder exercises illustrates this concept. The fault in strengthening weakened muscles through isolation training is that isolation training will fail to unify the painful or problematic joint with the entire locomotor system. Sure you can perform all the isolation exercises you wish, but this does not guarantee that the strength or coordination gained will automatically transform into adequate performance.
DNS exercises are applied in accordance with development kinesiology or essentially how we develop motor function during childhood. As we develop, reflexive movements (primitive, postural, locomotor) become more refined and coordinated, ultimately leading to specific movements we produce later in life such as walking, running, jumping, reaching, throwing, etc.
However, developing these skills does not happen magically. Learning to control the body and developing fundamental skills make up our motor milestones. These milestones mark critical points in our development and there is a progression that these milestones follow. This is known as developmental kinesiology. In simplistic terms, we need to be able to lift our head and support it, roll over, crawl, support ourselves upright, walk with assistance, and then walk without support.
The understanding of developmental kinesiology and critical motor milestones allows the provider to make exercise progressions and regressions during the course of therapy in order to appropriately address the underlying locomotor system dysfunction(s).
These exercises are applicable for patients with variety of acute and chronic conditions as well as for athletes who are trying to improve their performance and also prevent or rehabilitate injuries.
Often DNS exercises are conducted with active support from the clinician to insure that the patient maintains proper support and executes ideal movement. DNS exercises could include the use of stability balls or bands to further facilitate the desired response of the exercise. These exercises are not only used to improve the stability of the spine, muscle coordination, balance and strength, but also to increase the body’s awareness and sensory integration.
Conclusion
All of a sudden, conservative management and treatment of patients and training of athletes looks a lot different than what is traditional accepted.
DNS is not only a magnificent approach for preventing and rehabilitating pain syndromes in the movement system it is also becoming extremely popular in sports performance circles. The same ideal patterns that keep an individual out of pain also maximize the efficiency of the movements, which not only reduces risk of injury but improves performance.
When you consider the principles of DNS, it truly is not about what exercises we prescribe or what exercises we perform, but rather what we are actually getting from those exercises when we perform them that is important. DNS provides a system of evaluation and treatment which follows motor development, thus providing an effective way to help our patients get the most out of therapy and our clients get the most out of training.
Sources:
Dynamic Neuromuscular Stabilization & Sports Rehabilitation, Frank C, Kobesova A, Kolar P. Int J Sports Phys Ther. , 2013 Feb;8(1):62-73.
A case study utilizing Vojta/Dynamic Neuromuscular Stabilization therapy to control symptoms of a chronic migraine sufferer, Juehring DD, Barber MR. J Bodyw Mov Ther, 2011 Oct;15(4):538-41.
Cerebellar function and hypermobility in patients with idiopathic scoliosis, Kobesova A, Drdakova L, Andel R, Kolar P. International Musculoskeletal Medicine. , 2013, 35(3): 99-105.
Effects of shoulder girdle dynamic stabilization exercise on hand muscle strength., Kobesova A, Dzvonik J, Kolar P, Sardina A, Andel R. Isokinetics and exercise Science. , 2015;23:21-32,
Developmental Kinesiology: Three Levels of Motor Control i the Assessment and Treatment of the Motor System. Kobesova A, Kolar P. Journal of Bodywork and Movement Therapies., 2014;18(1):23-33.
The Prague School of Rehabilitation, Kobesova A, Osborne N. International Musculoskeletal Medicine, 2012;34(2):39-41.
Postural - Locomotion Function in the Diagnosis and Treatment of Movement Disorders, Kolar P, Kobesova A. Clinical Chiropractic, 2010;13(1):58-68.
Analysis of Diaphragm Movement during Tidal Breathing and during its Activation while Breath Holding Using MRI Synchronized with Spirometry. Kolar P, Neuwirth J, Sanda J, Suchanek V, Svata Z, Volejnik J, Pivec M. Physiol Res, 2009;58(3):383-92.
Postural Function of the Diaphragm in Persons With and Without Chronic Low Back Pain. Kolar P, Sulc J, Kyncl M, Sanda J, Cakrt O, Andel R, Kumagai K, Kobesova A. J Orthop Sports Phys Ther, 2012;42:352-362.
Stabilizing function of the diaphragm: dynamic MRI and synchronized spirometric assessment, Kolar P, Sulc J, Kyncl M, Sanda J, Neuwirth J, Bokarius AV, Kriz J, Kobesova A. J Appl Physiol. , 2012;42(4):352-62.
Importance of Developmental Kinesiology for Manual Medicine, Kolar P. translated from Czech Journal of Rehabilitation and Physical Therapy, 1996;4:139-143.
Surgical treatment and motor development in patients suffering from cerebral palsy, Kolar P. Translated from Czech Journal of Rehabilitation and Physical Therapy, 2001;8(4):165-168.
Long-Term Efficacy of Dynamic Neuromuscular Stabilization in Treatment of Chronic Musculoskeletal Pain, Bokarius AV, Bokarius V. 12th World Congress on Pain. Glasgow, Scotland. Aug 17-22, 2008. Presentation # PF225.
A case study utilizing spinal manipulation and dynamic neuromuscular stabilization care to enhance function of a post cerebrovascular accident patient, Oppelt M,Juehring D,Sorgenfrey G, Harvey PJ, Larkin-Thier SM. Journal of Bodywork and Movement Therapies., 2014;18:17-22.
More related reading:
https://gallagherperformance.com/solving-pain-influence-czech-rehabilitation-techniques/
Why Therapists Should Understand Strength
As a chiropractor that specializes in manual therapy and rehab protocols, I see patients dealing with a variety of problems. Now while the conditions can vary greatly, the common denominator that all my patients share is that they are either in pain or unable to perform a specific activity at a level they desire. Being able to provide a service to help people was exactly why I got into chiropractic and it is why I work to continually develop my craft and treatment philosophy. My treatment philosophy has helped to develop my system for how I go about evaluating and treating each patient that comes to me for help. As valuable as my education and residency has been to developing my treatment philosophy, the insight and knowledge I have gained on strength and conditioning as an athlete and coach has been equally valuable.
A great mentor of mine told me that with his background as a strength coach, he uses that background and mindset everyday with his patients. Some years later, I continually have a renewed appreciation for what he communicated in that statement because looking at my patients through the "lens of strength" can provide me with a refreshing perspective.
Why?
Simply put, strength matters. Strength has the ability to cover up dysfunction. Strength will directly impact movement quality. Strength will improve mobility or flexibility issues. Strength has tremendous ability to minimize or reduce overuse injuries. Strength becomes a focus in my treatment plans and the advice I provide my patients.
In my opinion, a major player in the outcomes of patient care is the quality of advice they receive. Much of the advice I provide is directed at my patient's current exercise routine. And, at times, the advice is very blunt. The type of advice that is often tough to swallow on their part because it means big changes
What does that advice look like?
Say you are dealing with low back pain that is worsened from repetitive flexion. You can’t tolerate bending forward to tie your shoes or get nervous just thinking about picking up something from the floor, yet you love your group exercise class that has you running through dozens of crunches, sit-ups, air squats, and wall-balls. Your back is not going to respond to any form of therapy until you remove the irritating factor (your group exercise class) and follow the advice of substituting in more appropriate exercises that promote a healthy back.
Say you can’t properly lift your arms overhead with ideal form and posture through the shoulders, spine, and hips. Now you want to participate in an exercise routine that includes Olympic lifts such as the snatch and overhead pressing. What you must understand is that you lack the prerequisites to perform loaded overhead exercises. This is why your shoulders or low back hurt after overhead pressing or performing a full snatch and you need to be advised accordingly.
Advice should be constructive, providing a solution. However, there is some advice that is simply unacceptable. The classic example of this is the runner who develops knee pain, decides to see a doctor and is told, "Stop running."
Unacceptable.
The solution is rarely that simple. Maybe that runner lacks movement control in joints in such as the ankles, hips, pelvis, and spine because they lack adequate strength in surrounding musculature. Maybe that should be addressed while their current running program is restructured according to their tolerances.
There are solutions and often those solutions involve strength development.
As a therapist, odds are in your favor that you are going to find a strength deficit that is playing into that runner's knee pain. Odds are in your favor that you are going to find that lack of strength is correlated with any number of common conditions.
Lack of strength is never solved by inactivity and prescribing rest. Strength requires the opposite. Strength requires focus, guided effort. Strength is a difficult pursuit and it requires that one knows what they are doing if you are going to coach the process.
On my end as a therapist, what becomes even more difficult to navigate is managing a patient who has his or her own personal trainer or strength coach. I always ask them what they are doing for "training," and most times my response is inwardly shaking my head. I don’t say anything, unless I’m asked. If I’m asked, then it is time to be brutally honest.
It is important to note that you shouldn’t just take exercises away, but substitute better ones. My job is to find the best exercise for the job. This is why developing a large exercise pool to draw from is invaluable as a strength coach and as a rehab specialist. Having a huge exercise pool will allow you to make progressions, regressions, and substitutions based on movement patterns, training goals, mechanical sensitivities, or movement limitations.
At GP, we have taken time to develop our exercise pools for lower body pushes/pulls, upper body pushes/pulls, hybrids, developmental stabilization, etc. This allows seamless transition between phases of rehabilitative care for my patients and continual development from a strength and performance perspective for my athletes because we have developed our plan for progressive development. This understanding of strength also allows me to provide the most appropriate advice when it comes to exercise selection.
As William Penn said, “Right is right even if everyone is against it, and wrong is wrong even if everyone is for it.” People are there for your expertise and knowledge as much as your skills. Remember to provide the care and treatment you would want to receive and provide them with the advice and direction you would want to understand.
More related reading:
https://gallagherperformance.com/interview-with-mike-odonnell-dc-ccsp-cscs/
https://gallagherperformance.com/the-best-exercise/
https://gallagherperformance.com/before-you-go-to-a-chiropractor-read-this-first/
Interview with Ben Gallagher DPT, FMSC
GP recently interviewed Ben Gallagher DPT, FMSC. If you happened to figure out that Dr. Ben is related to us, you are correct. Ben is a physical therapist at Somerset (PA) Hospital Rehabilitation and Wellness Center. As brothers, we share some very similar concepts in the treatment of patients. But, we also share contrasting viewpoints, which makes it fun to learn from each other and gain a better understanding of the professional roles we serve in providing improved quality of patient care.
Now, let's get to the questions.
GP: Please introduce yourself and give our readers some information on your professional, educational, and athletic background (as well as what you have had to overcome since birth in order to participate in athletics).
BG: My name is Ben Gallagher, brother to Sean and Ryan. I live in Somerset, PA with my wife and daughter. I am a physical therapist and have been working at Somerset Hospital Rehabilitation and Wellness Center for over two years. I graduated from Indiana University of Pennsylvania (IUP) with a degree in Exercise Science in 2008. Then went on to Saint Francis (PA) University to get my Doctorate in Physical Therapy, graduating in 2012. Since graduating I have become FMS (Functional Movement Screen) certified, focusing my continuing education on movement analysis and manual therapies thus far.
Athletically, I grew up playing most sports, mainly focusing on basketball until the 8th grade when I got into ice-hockey as a goaltender, then that became my passion. I played through high school and into college at IUP. As for what I had to "overcome," that would be referencing my heart condition. I was born with Tetrology of Fallot, a congenital disorder that required surgery as a young child and again in 2008, and another in about 15-20 years. The condition restricted me from some sports and it is not advised I lift max weights, placing a limitation of how I could physically train for sport. However, prior to my 2008 surgery, in which my heart was over 3x normal size, I had no issues or symptoms. The doctors attributed my training to why I could function so well with such a crappy heart. Training was a mainstay, and still is.
GP: The thought process in your evaluation and management of patients is not widely instructed in physical therapy programs. What were the biggest influences in your professional development in not only the care that you provide, but also why you sought out additional resources beyond what you learned in school?
BG: The purpose of physical therapy school is to: 1) make sure you pass the licensure exam, and 2) make sure you don't seriously hurt anyone. As for producing quality clinicians? No. School just teaches you the basics, and most practicing therapists provide you just that, the basics, which is what you could find on a Google search. So, as for what helped my professional development, honestly the biggest thing was I just thought differently. I saw things differently and I attribute that to my athletic background and training history. For example, as a PT student I would tell my class-mates, "I'm gonna have my grandmas deadlifting." My classmates would gasp, as if that was the most absurd thing they ever heard. But my thinking was, "If someone needs to build strength, why am I gonna have them lie down and lift their leg? When I want to build strength, I train the squat and deadlift, so how couldn't the same application benefit my patients?" Now let me clarify, not all movements are appropriate for all people, at all times. That's why programs need to be individualized, not cookie-cutter.
So for me, I thought, why do I want to further inundate myself with PT knowledge that is elementary and narrow-minded. I sought out other means to fill that thirst for a fuller, better understanding of how the body functions. FMS, which is for any health or fitness professional, is just one of many means to that end that I am pursuing.
Plus, I have to add this: In reference to the grandmas deadlifting story, there was a research article published shortly after in regards to the most effective exercises to strengthen the hips. The study basically ridiculed all traditional PT exercises and found the most effective was a single-leg deadlift. How 'bout them apples?
GP: You are extremely involved with your patient’s care, preferring to perform a lot of manual therapy and oversee the exercise process. This is not common of the majority of physical therapists. Can you speak to why you find this so valuable in the outcomes your patients are able to achieve?
BG: I don't even know where to begin with this issue. I get fired up about the lack of quality care there is in this field. Most therapists treat with a shot-gun approach, meaning they're not sure what is really going on or how to treat so they will throw a ton of stuff at you hoping something sticks and works. But the best in rehab are like snipers. They isolate what the exact issue is and address it appropriately. And how can you do that if you are not present and in the mix with your patient's rehab process?
GP: As a physical therapist, you see tremendous value in what chiropractic care has to offer. Could you please give your thoughts on what makes chiropractic and physical therapy so complementary?
BG: Following off the above question, when you are involved with your patient's care, you may find that some issue(s) may be out of your scope and there may be better, more skilled hands that are able to provide effective care. How can one means of healthcare be the most effective? What is most effective is what the patient needs. How can chiropractic care be so bad, which is the view of many therapists, when chiropractors help so many? And how can therapists think we are the kings of rehab and exercise when many therapists stick you on a machine and walk away? I have referred patients to chiropractors and massage therapists. But, I do so instructing them on what they need to share with those professionals, because just going blindly to another professional does not always mean you will get quality care. Chiropractor, massage therapist, physical therapist, strength coach….I don't care what your title is; if you're good, you're good.
GP: Posture, stability, and mobility are intensely debated topics at conferences and continuing education seminars. Could you expand on your philosophy when it comes to the dynamic role between posture, stability, and mobility, what athletes and coaches should understand about these topics, and what should be left to physical medicine providers such as physical therapists and chiropractors?
BG: The first thing that athletes and coaches should understand about posture, stability and mobility is that you likely don't fully understand these concepts. Most lay people honestly don't understand how posture impacts how their body feels and the role it has in movement. Someone with good posture likely can't explain why they have good posture or how they achieved it. But, that is why we, as professionals, are here.
The stability-mobility debate is like a left-wing versus right-wing debate. My philosophy is it's a spectrum. No one physical issue is 100% in either direction, but I do believe stability is the issue the majority of the time. And if mobility is an issue, and is addressed, such as stretching or mobilizing, it should complimented by stabilization training to ensure you have control of the new motion you have just obtained.
GP: You have developed a reputation in your area as a “go-to-therapist” for athletes being referred from orthopedic surgeons because of your eye for assessing movement and your ability to successfully return athletes to competition. Besides the FMS, what other assessments do you find valuable in dealing with athletes and their competition needs?
BG: For those who don't know, the FMS is a tool used to assess a person's quality of movement using seven standardized movements. If you move poorly, you are then going to compensate, compensation leads to altered or poor biomechanics, which leads to injury. So the whole purpose of the FMS is to make sure you move well. The job of the clinician is to not only identify poor movement, but to also figure out why you are not moving well. Therefore, what other assessments do I find valuable for athletes? I want to see them go through their athletic movements: swing a golf club or hockey stick, throw a ball, jump, land, cut, sprint, run, etc.
To be able to do this effectively you must first be able to analyze the movement correctly. Is the movement efficient? If it is not, then you must be able to figure out why it is not and be able to address the problem effectively. All this said, what is really needed is knowledge of athletic movement, a good clinical eye, and the knowledge of how to fix whatever issues are present.
That’s a Wrap
Ben, thank you for taking the time to answer our questions. Your knowledge and insight is truly appreciated. We hope this was informative for our readers as well. For those in the Somerset, PA area, be sure to check out Ben at the Somerset Hospital Rehabilitation and Wellness Center for tremendous results when it comes to returning from injury or understanding how to move better for your exercise or sport-related goals.
More related reading:
https://gallagherperformance.com/posture-and-movement-linking-training-and-therapy/
https://gallagherperformance.com/prevent-re-injury-integrated-training-rehabilitation/