[embed]https://www.youtube.com/watch?v=pmkt-yv3JZ0[/embed]
Nothing beats properly performed squats, deadlifts, lunges, and RDLs for glutes that not only look great but work even better. Proper glute function is critical to hip extension that is prevalent in every day life (walking, sit to stand, hip hinge, lifting) as well as sport (running, sprinting, throwing, jumping, skating) Problem is most people don’t perform the big exercises well and therefore resort to ways to “activate” or better “isolate” glute function. This is why hip thrusts exist. They have their place when used with a plan and purpose. The single leg hip thrust is an advanced progression that is often performed incorrectly. The biggest mistake being the unleveling of the hips that can occur during the movement. By using the external cue of a tennis ball, we can promote better technique that results in improved muscular coordination of the glutes and core. This translates into more efficient movement mechanics, not only in this exercise, but in life and sport as well. Hopefully the video explains the set-up and execution well enough for you to give it a try.
For more related reading:
https://gallagherperformance.com/resetting-bodys-function-post-injury/
https://gallagherperformance.com/dns-solves-pain-improves-performance/
https://gallagherperformance.com/the-essentials-of-hamstring-rehab/
https://gallagherperformance.com/the-best-exercise/
Posture & Movement Require Brain Education
Our brain controls our posture and our muscles. Therefore posture and muscle tone (i.e. how tight or relaxed a muscle is) is an expression of the brain. We must pay attention to this expression and how it relates to movement.
A frequent cause of disturbance in our movement quality, why muscles get tight, why we display poor posture, and why we may have trigger points or pain is due to insufficient muscular stabilization of our spine.
Insufficiency is our stabilization system is exactly the reason why patients and athletes who have poor body awareness demonstrate poor ability to simply relaxation. Believe it or not, relaxation is easier said than done. If the brain doesn't know how to relax fully certain muscles, the low-grade state of contraction will keep muscles and surrounding joints under constant stress. This constant stress will ultimately lead to trigger points in muscles, dysfunctional movement patterns, and altered posture.
This is why specific exercise progressions that respect the developmental aspects of posture and movement are so critical. Exercise should not only address muscle function, but it must also address brain control to change how our body functions.
"Brain Education" focuses on the efficiency of our postural and movement control to avoid overloading of specific tissues and joints while promoting muscular balance.
Movement and relaxation is a skill. It must be practice daily through purposeful exercise with complete awareness to the feeling of the movement. This is the gateway to change in the body. These changes are valuable to anyone who is simply looking to get out of pain or improve their athletic ability.
However, there are still those that challenge the notion that there is an “ideal” or “good” posture. They will have you believe that there is no such thing as “good” or “bad” posture. The reality is, when it comes down to determining what is “good” or “bad” posture can be simply summed up by saying….”It depends.”
What will dictate “good” or “bad” when it comes to form or posture will depend upon a number of variables specific to the individual. We can find efficient form and ideal posture that someone should respect and when they don’t, the result is excessive wear and tear on their joints and tissues, leading to pain and progression of degenerative changes.
Yes we need to be efficient in movement and have a vast movement capacity. Yes there is no single posture that we should maintain for an extended period of time, no matter how “good” it is.
But those notions go out the window when our body meets increasing external resistance to our movement or we are performing movement at increasing speeds.
What does that mean?
Yes, we should be able to flex our spines and perform a body weight squat with posterior pelvic tilt (aka the dreaded “butt wink”) and resultant lumbar spine flexion. Yes this would be considered normal healthy human motion. But that doesn’t mean that one should perform a loaded barbell squat with the same intent or form. This could be an injury waiting to happen. When increased load or speed of movement comes into the picture (ex. barbell squat), very specific considerations must be made to that individual on the form and posture they express during the squat pattern to maximize their muscular efficiency and minimize stress placed on the joints.
These are the same considerations that must be respected when it comes to rehab and the subsequent development of fitness/physical ability. According to McGill, this breaks down into two stages:
- Stabilization of the injury and reduction of pain by approaches that follow desensitization and healing.
- Development of strength and physical ability only begins when the first stage has been achieved.
Once pain is reduced, the development of specific fitness qualities can take center stage. This is when we address the complexity of the movement system. Panjabi established the importance of the passive, active, and neural systems for trunk/core stability and movement. Jull and Richardson found in voluntary movement, activity of the deep spinal muscles precedes activations of the superficial muscles (aka feed forward mechanism).
The integrated spinal stabilization system (ISSS) serves as the “feed forward stabilization mechanism”. The ISSS consists of the diaphragm, pelvic floor, all parts of the abdominal wall, short intersegmental spinal muscles, deep neck flexors, and serratus anterior. We know that these muscles essentially form the “deep core” that is so important to train for efficiency of posture and movement.
The ISSS required “Brain Education” to work optimally. There is no way around it. We must focus our attention and efforts to ensuring that no matter the task, we must rely of the ISSS if we are going to realize our movement potential, maintain healthy posture, and minimize joint pain.
Don’t fall into the trap of believing someone who says “good” or “bad” posture doesn’t exist. Again the answer is it all depends. Posture and the considerations we make regarding it are always specific to the individual and task at hand. Posture shouldn’t handled in a general approach. Most rehab, training programs and online instruction is handled in an over-generalized fashion. When people need specific, when they need individualized considerations. And that’s the best approach when it comes to helping one learn how to educate their body in regards to what’s best for their posture and movement.
For more related reading:
https://gallagherperformance.com/movement-that-enhances-performance-reduces-injury/
https://gallagherperformance.com/a-movement-screen-will-never-show-movement-habits/
https://gallagherperformance.com/low_back_pain_causes_and_treatment_recommendations/
https://gallagherperformance.com/chiropractic-rehab-dns-treatment/
https://gallagherperformance.com/a-solution-to-headaches/
https://gallagherperformance.com/finding-a-solution-to-your-shoulder-pain/
The Essentials of Hamstring Rehab
[embed]https://www.youtube.com/watch?v=oZUKOz1iuhk[/embed]
This video highlights the hamstring rehab with Carter Henderson. Carter was a standout linebacker at Duquesne University, leading the team in tackles the last two seasons. Now he is in preparation for an NFL Pro Day.
Carter came to GP for rehab of a hamstring pull 12 days out from his Pro Day. His initial 5 days focused on manual therapy, eleetromuscular stimulation (EMS), with a primary emphasis on exercise progressions based on his tolerances and weaknesses. Focus was placed on exercise specificity to the stresses the hamstrings encounter during sprinting. We aimed to match joint angles, mechanics, and dynamics as they relate to his sprint form and lateral movement.
Days 6-8 on his rehab focused on tempo runs and flying 40s, keeping intensity below 75% effort. Gradually worked into higher intensities with specificity to pro day drills. Focus still on manual therapy, joint mobilizations and manipulation when indicated.
Effective treatment for a hamstring strain, and for any injury, must address not only the site of pain but ALL possible predisposing factors. There are essentially three ‘reasons’ as to why hamstring injuries occur. Sprinting is not the problem. Focusing on each predisposing factor through progressive treatment and training will best prepare the athlete for return to sport activities.
The act of ‘pulling’ a hamstring usually occurs at high speed running during the terminal swing phase of the gait cycle. As the hip is decelerating the forceful momentum as the leg swings forward, the hamstrings are loaded and lengthening as you are finishing the swing phase before foot strike. There are predisposing factors that ultimately cause the hamstring to be compromised such as:
- Poor neuromuscular control of the lumbopelvic region,
- Asymmetries in muscle length and/or hip range of motion, and
- Sacroiliac joint dysfunction
The utilization of manipulation, massage, soft tissue techniques, and nutritional considerations to support tissue healing become the foundation of early care and recovery from hamstring injury. Everything used to facilitate healing is based on examination and identification of the presence of any predisposing factor(s).
The transition from rehabilitation to return to sport then becomes dependent upon a process that addresses proper tissue healing and exercise progressions to improve structural balance, lumbopelvic control, strength, and coordination of movement required by sport specific demands in output and movement patterns.
This essentially sums up the process behind Carter's rehabilitation program.
Carter has turned around nicely and tons of credit to him. He wasn't able to walk without pain when we first started his rehab and was able to run a 4.75 sec 40 yard sprint on his pro day at Duquesne University. He did everything right in his rehab. Carter is extremely coachable and great to work with and we wish him all the best.
For more related reading:
https://gallagherperformance.com/solving-pain-influence-czech-rehabilitation-techniques/
https://gallagherperformance.com/posture-and-movement-linking-training-and-therapy/
https://gallagherperformance.com/makes-sports-rehabilitation-chiropractor/
https://gallagherperformance.com/fascia_muscular-adhesions_how_they_relate-_to_pain_and_overuse_injuries/
https://gallagherperformance.com/best-way-recover-tendon-pain/
A Movement Screen Will Never Show Movement Habits
Movement screens or testing can offer valuable insight into why you have pain or limited function.
However what tends to be more valuable is when someone help you understand your movement habits.
By observing how someone moves and the postures they assume during daily activities - walking, bending, twisting, reaching, pushing, or pulling - we can tell you more about the chronic stresses that may be the major contributors to your current problem.
Without understanding your movement habits, we are missing a big part of the healing process or why you experience plateaus in your training/exercise program.
Once you understand movement habits the focus becomes finding what provokes your pain and discovering your weaknesses. By identifying pain triggers, we can build a plan that enables you to control your pain and improve function while your body heals.
Systems and screens for movement are a useful tool, but they tend to be general in nature. They aren't highly specific to the individual all the time. They might work, but often times you must dig deeper and be more accurate in observation, evaluation, treatment, and self-management to help someone achieve their goals.
https://gallagherperformance.com/3-common-reasons-low-back-pain/
https://gallagherperformance.com/dynamic-duo-chiropractic-dns/
https://gallagherperformance.com/resetting-bodys-function-post-injury/
https://gallagherperformance.com/powerful-innovative-approach-improving-body-functions/
https://gallagherperformance.com/tendinitis-changing-treatment-and-improving-recovery/
15 Minutes of Exercise OR 8+ Hours of Pain?
Just because you are in pain or injured does not mean you are fragile. Patient advice, education, and treatment that carries an over reliance on rest, ice, immobilization, and drugs only promotes fear-avoidance behaviors in patients - leaving them feeling fragile. What they need instead is graded exposure and reactivation to physical activity through movement re-education, strength training, and re-conditioning.
Research and clinical guidelines are consistently supporting exercise as THE number one intervention for back and joint pain.
Exercise provides the best long term outcomes. Sadly most people are never introduced to proper exercise for their back/joint pain OR would rather simply mask their pain symptoms with a drug, brace, tape, or some sort of passive modality yet they wonder why their pain continues to return.
These interventions have their merit, I'm not dismissing them as useless. However, when there is an over reliance upon these interventions without a shift in focus to graded exposure to physical activity through movement and exercise - it is easy to conclude why some people fail to get out of pain.
It's one thing to change pain, it's another to change how the body functions and impact the reasons WHY you developed pain in the first place. If you don't change function, this is the reason why patients relapse often.
Exercise become our gateway to change in the body. Exercise is treated like a drug in terms of dose and response. We need to dose (i.e. how much, what kinds, how often) exercise appropriately in order to get the ideal response (i.e. reduced pain, improved function).
Proper movement and smart exercise is the best medicine so let's dish it out!
You can accomplish more than you can imagine in just 15 minutes of daily, targeted exercise that is intelligently implement to address your weaknesses and eliminate your pain generators. Or the other option is to spend the majority of your day in pain, implementing questionable interventions that will do little to solve your problem in the long term.
Exercise should be viewed as a means to improve your quality of life. A means to make every day activities easier on your body. Or a means to improve function and therefore improving endurance, strength, power, and athleticism.
If you are ready to eliminate pain, erase weaknesses, improve how your body functions, or simply get in the best shape of your life - Gallagher Performance will get you on the right track to achieve those goals.
More related reading:
https://www.gallagherperformance.com/blog/a-powerful-innovative-approach-to-improving-how-the-body-functions
https://www.gallagherperformance.com/blog/tendinopathy-changing-treatment-and-improving-recovery
https://www.gallagherperformance.com/blog/how-movement-improves-brain-function
https://www.gallagherperformance.com/blog/how-dns-solves-pain-and-improves-performance
Exercise Hacks Ep. 11 - Train the Abdominal Slings for a Functional Core
[embed]https://www.youtube.com/watch?v=YybcsllEkhk[/embed]
Two common sites for pain and movement problems are the low back and sacroiliac (SI) joints. The SI joints are a common site for sensitivity due to biomechanical overload.
Once we have screened for sensitivities, pain generators and movement dysfunction, the presence of SI joint dysfunction is often found along with poor abdominal sling function. Chiropractic adjustments are great for addressing joint dysfunction, but we must train movement through specific exercise.
Addressing abdominal sling function is critical as the SI joints receive stability from the force closure our musculature provides. Poor function of these abdominal slings results in poor stability (and often pain) in the SI joints during walking, running, squatting, lunging, bending, pushing or pulling.
Our abdominal slings are present on the front (anterior) and back (posterior) of our core. The anterior sling being made of the pec major, external oblique, internal oblique, and transverse abdominus. The posterior sling being made of the latissiums dorsi and opposite glute complex.
These exercises demonstrate how to strengthen the abdominal slings as a functional unit. You want to think transverse plane.
Cable chop variations are great for the anterior sling. Cable chops are excellent for building a functional anterior sling for stability and efficient force transfer, especially for front side mechanics as it relates to running, sprinting, jumping, and throwing.
The posterior sling can be targeted with Single-leg Romanian deadlift (RDL) variations as shown. Drawing tension through the lats and glutes provides the stability in the posterior sling to improve motor control of the lumbopelvic region for efficient hip extension. Clean, efficient and - at times - powerful hip extension is critical to a number of athletic movements as well as daily living.
Our hips should be the "King of Motion" in the body, yet many of us deal with tight hips and painful backs or SI joints as a consequence. Our hip movement must be trained and optimized, but the hips will only be as efficient as the abdominal slings allow.
Give these exercises a shot. Let us know your thoughts or questions!
For more related reading:
https://gallagherperformance.com/beginners-guide-injury-recovery/
https://gallagherperformance.com/improved-approach-chronic-pain-management/
https://gallagherperformance.com/3-exercises-athletic-mobile-hips/
https://gallagherperformance.com/exercise-hacks-ep-8-breathing-bracing/
https://gallagherperformance.com/do-you-really-need-more-mobility/
Are You Receiving Value in Your Treatment or Training?
The combination of chiropractic/manual therapy and massage therapy paired with smart training can make a profound impact on any musculoskeletal condition you may be dealing with. There's tremendous value in care and training that focuses on the goals and outcomes you care about. You place a value on your health or performance and you should receive services that deliver value.
The challenge is finding a chiropractor, therapist, or trainer who aligns with your values and the value that you place on your body and health. There's a spectrum on which these providers exist and it becomes your responsibility to do your homework. To make sure you find someone that can deliver the care, quality, results, and value that you're looking for.
You can go to 10 chiropractors and have 10 totally different experiences. You could see 10 personal trainers and have 10 totally different experiences. Yet all those experiences fall under the broad categories of 'chiropractic' or 'personal training'.
You don't know what you're getting into until you do some research and understand how someone practices or how they are going to approach your specific exercise program.
Some may argue one way may not be better than another way, but there are certainly more affective means of treatment and training that get better results.
There is a responsibility on the individual to find someone who will deliver that value. People often go through detailed vetting processes when it comes to a mechanic, electrician, plumber, doctor, etc. When it comes to your health, are you vetting the people you work with?
A big reason why we get a lot of athletes and individuals that prioritize their health is they do their homework. They want to understand how the body works and they are driven to optimize it. They search out the right person for the job. They want someone to deliver value in the care and the training that they are receiving because they realize they only have one body and they want to take care of it to the best of their ability.
Are you placing value on your health, fitness, or sport goals? Or are you just looking for the best price?
More related reading:
https://gallagherperformance.com/the-best-exercise/
https://gallagherperformance.com/essentials-of-keeping-athletes-healthy/
https://gallagherperformance.com/options-dont-take-insurance/
https://gallagherperformance.com/the-benefits-of-performance-therapy/
https://gallagherperformance.com/powerful-innovative-approach-improving-body-functions/
Stop Chasing Shortcuts
When it comes to health, fitness, or athletic goals, there is no secret. There is no special exercise class, no special equipment or supplement. There is no magic. Yet people keep looking for one.
The truth is there are no shortcuts and anyone promoting shortcuts is lying to you. And if you bought it, you were buying 'hope' only to discover you actually got a bunch of nonsense that left you disappointed and frustrated.
Chasing shortcuts is a mentality that is robbing people of not only achieving their goals, but the ability to maintain them. If you some how think that serious health and fitness goals are able to be achieved with anything less than 100% commitment, dedication, discipline, and will power to sacrifice for your goals - there is nothing anything or anyone can magically do for you.
Spend your time, energy, and resources on what does work instead of chasing shortcuts. Recognize the work it is going to take and commit 100% to your goals.
Is this easy? No way. Most want something only when it's convenient or when it's easy to prioritize. They prefer the sound of some shortcut that will get them where they want to be - with less effort, less time, or without changing anything.
Where are you getting advice? Who are you listening to? Are they simply trying to sell you a BS program or product? Stop listening to this nonsense. It doesn't work. What works is tried and true sustainable actions with long-term focus.
Sustainable actions may be tedious and boring. But you know what isn't boring? The results sustainable actions consistently produce and the ability to maintain them. Ask anyone that's ever achieved anything worthwhile - in business, academics, or athletics - they all found success in doing the tedious and boring. All day. Every day.
Health. Fitness. Performance. Nutrition. They're no different. They are all lifetime pursuits. It's called a 'lifestyle' for a reason -you have to be in it for life. The question is do you value your goals enough to commit to the level of work, dedication, discipline, and will power needed to achieve them?
Change your mindset. No excuses. No shortcuts. Just results.
More related reading:
https://gallagherperformance.com/what-is-natural-talent/
https://gallagherperformance.com/attitude-is-everything/
https://gallagherperformance.com/learning-through-misconceptions/
https://gallagherperformance.com/training-tip/
https://gallagherperformance.com/dns-solves-pain-improves-performance/
Exercise Hacks Ep. 10 - Loaded Progression for Shin Box Get-Up
[embed]https://www.youtube.com/watch?v=WwIba7PpgXA[/embed]
Keeping with the concept of core stability and hip mobility, the shin box has become a popular drill for improving hip rotation, eccentric loading of the hips, as well as reinforcing ideal intra-abdominal pressure (IAP) and core stability.
Ideally the shin box is performed in a progression of static to dynamic variations. Progressions are dependent upon the ability to achieve ideal external rotation in the lead leg and internal rotation in the trail leg while maintain an upright, braced torso with sufficient IAP.
While the shin box and its get-up variations are most popularly used as a warm-up/movement prep or 'mobility' drill, loaded progressions can be an awesome tool for increasing hip strength and neuromuscular coordination of force transfer through the hips and core.
This advanced progression of the shin box involves the hanging band technique with a safety squat bar. The hanging band technique is great for cleaning up technique and reinforcing proper stability and motor control. Failure to control your technique or movement will result in the hanging weighs to sway uncontrollably. The fight your body goes through to maintain stability and the control needed to avoid excessive sway does plenty to 'coach' one how they should be moving. There's tremendous value in utilizing exercises or movements that allow one to problem solve on their own. That's what makes this loaded progression an awesome tool.
Not only are you improving 'mobility' but you're also developing strength and doing so in a way that movement quality won't be compromised because of load. It's something that happens all too often with exercise. You see people sacrificing form and quality of movement for the sake of more weight on the bar. With this exercise it isn't going to happen. If you try to perform this exercise with too heavy a load that causes form breakdown, the movement isn't happening at all. Arguably, one of the biggest contributors to 'mobility' issues is poor form associated with mismanaged loading strategies - or basically trying to 'muscle through reps' at the expense of quality in movement. This ultimately will cause joint issues and mobility restrictions as you place too much stress on your joints on a repetitive basis.
So what's the best solution to mobility issues?
Sometimes the best mobility drill is building the foundation of ideal technique in a well-designed strength training program that erases your weakness. And this loaded progression of the shin-box get-up does just that.
For more related reading:
https://gallagherperformance.com/do-you-really-need-more-mobility/
https://gallagherperformance.com/solving-movement-problems-entertainment-vs-effective/
https://gallagherperformance.com/the-best-exercise/
https://gallagherperformance.com/unlock_your_potential_with_this_powerful_tip/
5 Reasons Not to Be Skeptical of Chiropractors
You've thought about seeing a chiropractor before, but have hesitated because you:
- Heard it was "BS" or "quackery"
- Thought that once you start going, you'll have to go for life
- Were afraid of being adjusted
- Thought they just won't be able to help
In fact, chiropractors have the ability to successfully treat a number of common musculoskeletal problems. Below you will find five reasons why you shouldn't be so skeptical of chiropractors and why finding a great chiropractor can prove to be a priceless investment to your health and well being.
1. Solve joint and muscle pain without unnecessary medication or surgery
Let's illustrate the significance of this point with an all-too-common experience for many of us. You begin to experience joint (neck, back, shoulder, knee, etc.) pain seemingly for no reason at all. Your pain has just appeared and you are puzzled as to why.What do must people do first?
Most commonly, they start in the medicine cabinet with common over-the-counter (OTC) medications like Tylenol, Motrin, Advil, or Aleve. They may ice the area or apply pain-relieving gels. Others may just give it time and play the waiting game to see if the pain goes away on its own. If OTCs, ice, pain-relieving gels or time don’t do the trick, then they pay a visit their primary care physician only to receive a script for either anti-inflamatories or muscle relaxers and a referral for an orthopedic consult. The orthopedist will likely perform a physical examination along with possibly ordering imaging studies such X-ray, CT scan, or MRI. Based on your examination and imaging results, one of two recommendations is often made - physical therapy or surgery.
Too often surgery can be recommended before more conservative approaches are given a chance. Disregarding the risks associated with surgery, what happens when the procedure fails? Surgery is not a great choice when pain is associated with a positive — often incidental — finding on an MRI. These incidental findings are well document and often times structural adaptations to functional problems.
When assessed properly by a trusted conservative musculoskeletal care specialist, whether a chiropractor or physical therapist, many muscle and joint problems can be resolved without the need for surgery.
Seek conservative care first. If you don't respond to care within 6 weeks, then it wish to consider more invasive procedures if they are indicated.
2. Manage complicated disorders
Remember when I said all chiropractors are different? It's true.Just like the medical profession, there are many areas of specialty in chiropractic. Those who specialize as a sports injury & rehabilitation chiropractor (such as Dr. Gallagher) have undergone the traditional education on joint manipulation or adjustments. However, in addition to their core curriculum, sports injury & rehabilitation complete hundreds of hours in continuing education learning about exercise and sport-related injuries, manual therapy, and functional rehabilitation methods.
Chiropractors who utilize a sports injury & rehabilitation approach incorporate joint mobilization/manipulation, soft-tissue treatments, various manual therapies, and functional rehabilitation techniques to provide a gold standard of care in treatment for individuals with exercise and sport-related injuries. This combination of complementary approaches uniquely positions sports injury & rehabilitation chiropractors to manage complicated disorders that other specialists may have difficulty in treating.
3. Prevent future episodes of pain by changing function
Imagine a world where patients get the advise, education, and treatment they need. Imagine doctors who:- Make sense of what a patients says
- Know exactly what a patient needs
- Confidently provide gold standard advice and treatment interventions
As ac chiropractor it's my job to educate my patients and help them problem solve. I have to help them understand not just what their problem is, but more importantly why it started.
In understanding why their problem started, we aim to change the function of their body. If patients don't commit to changing their behaviors and habits that got them into pain in the first place, then how can they expect to find a solution to their problem?
4. Enjoy a healthier lifestyle
As stated in the point above, chiropractors should be educators. As educators, we teach individuals how to live their best life and do so in a model that promotes our patients's have a sense of independence, capable of making informed, intelligent lifestyle choices.Regardless of specialization, a universal truth to chiropractors is that they generally practice a “holistic” approach to patient treatment. Meaning chiropractors view the individual as a whole, identifying and focusing on more than just physical symptoms such as pain. By employing a combination of manual treatments, ergonomics, postural education, exercise prescription, nutritional interventions, lifestyle advice, and other strategies (practitioner dependent), chiropractic is more than just cracking backs to reduce pain. Chiropractors want their patients to enjoy a healthier lifestyle.
5. Enhanced performance
We put our bodies through the ringer daily (some more intensely then others). Periodic treatment from a qualified chiropractor will help keep your body running like a fine-tuned machine, improving your ability to perform and progress in your training programs by optimizing the body’s ability to function at it’s best.How?
By combining chiropractic with functional rehabilitation and strength and conditioning principles.
It's exactly why we do what we do at Gallagher Performance.
Almost every case involving muscle or joint pain requires some level of strengthening exercise progression and education. We will make sure you are doing the most appropriate exercises for your situation and your level of ability. By clearly educating each patient on why they are performing their prescribed exercises or stretches, the focus becomes about patient empowerment and providing them with a sense of what they can do for themselves to keep pain from returning.
Regardless of the number of treatments you receive, the goal remains the same – to make a lasting change in your body through posture and movement re-education.
Wrapping Up
There are many great reasons to visit a chiropractor. Every chiropractor is different, so just because one didn’t work for you it doesn't mean that all chiropractors are useless. You just haven't found the right one for the job and that can prove to be a difficult task. Yes there are some bad ones out there (like any profession), but there are plenty of good ones that can be trusted.No matter who you see, keep in mind that it is critically important that you understand your problem, your treatment plan, your expectations for recovery, and how to manage your problem during as well as after treatment.
At Gallagher Performance it is our intent to get you back to what you love doing and as quickly as possible. We create clarity by helping you understand your problem, why it behaves they way it does, and apply the right tool to make a lasting change in the way your body functions.
More related reading:
https://gallagherperformance.com/dynamic-duo-chiropractic-dns/
https://gallagherperformance.com/busting-chiropractic-myths-misconceptions/
https://gallagherperformance.com/are-you-promoting-independence/
https://gallagherperformance.com/before-you-go-to-a-chiropractor-read-this-first/
https://gallagherperformance.com/when-should-i-see-chiropractor/
Dynamic Duo - Chiropractic and DNS
When it comes to Dynamic Neuromuscular Stabilization (DNS), those that are familiar with the method will often ask me, "How do I find the time to treat my patients with chiropractic, rehab methods, and DNS?"
The reasons for the question is simple - DNS is seen as very time consuming. The challenge with DNS is incorporating the method into a busy practice while remaining efficient and delivering a high level of quality care to your patients.
It's a difficult scenario for me to connect with since I have always maintained a schedule which enables me to spend 30-60 minutes with each patient. However, I realize this is not the norm for the overwhelming majority of chiropractors and they are under more of a time crunch to deliver the most they can in a shorter period of time. Even most physical therapists I know do not have that time to spend with a patient 1-on-1 as they normally have a number of patients blocked together for appointments and rely upon help from their assistants.
That said, the reality is until one has been properly trained in DNS, they will continue to assume that the amount of assessments, patient education, instruction, and exercise-based interventions will all add up to extra time with patients they simple don't have.
In my opinion, the time I have taken to study, learn, and implement DNS concepts into my patient care has only been a compliment to what I do as a chiropractor. Chiropractic, in a very traditional sense, is the healing art based on the science of the nervous system and it's relationship to altered spinal joint mechanics. At its very root, chiropractic aims to improve the functional of the nervous system through manual methods or manipulative therapy of the spinal joints. There is a tremendous focus on the musculoskeletal system and its relationship to the health of the nervous system. Chiropractors evaluate for postural, structural, functional, and movement-based imbalances that play a role in either pain, dysfunction, or reduced expression of overall health.
As a chiropractor, we routinely treat patients to get them out of pain, but we also work with them to restore health and a quality of life they want to maintain. And that's what makes chiropractic and DNS such an awesome combination. They both produce results that enable patients to get out of pain, improve function, restore health and get back to enjoying their life.
As a chiropractor, I use DNS assessments to identify movement patterns that are non-ideal in regard to stability and mobility. DNS is not merely a technique, but rather an overall strategy to better understand the principles of movement. It includes both a knowledge and theoretical base that forms the foundation for assessment, treatment, exercise and functional strategies.
We aren't simply just looking for joints that don't move well or muscles that are too tight or weak. The focus of DNS is correcting faulty movement patterns that ultimately cause tight or weak muscles and joint fixations. By performing basic assessments it is possible to identify what the problems are and what exercise interventions would successfully achieve the desired correction - and this can all be done quickly. This biggest misconception is that providers need to instruct their patients in a large number of exercises in order to correct dysfunction in movement stability or mobility. This couldn't be further from the truth. My patients only perform the most challenging exercises with the proper stabilization and movement control. This means that most patients are leaving with 2-3 home exercises and there are those that will leave with only one exercise.
These exercises are intend to improve the sensory messages our brain receives from movement. We can thank the modern sedentary lifestyle and simply not moving with enough variety for the decline we see in maintaining a healthy brain and nervous system. This decline presents itself in postural abnormalities and altered movement patterns And both can be addressed through exercises and improved proprioceptive control of our joints and movement.
The exercises are intended to be functionally-based and proprioceptively-rich. This enables the patient to create a lot change from just from a few exercises - training economy at it's finest. When it comes to DNS exercises, patients get a great deal of results without having to invest a lot of time.
Furthermore, chiropractic adjustments improve sensory inputs from the spine to the brain and this proprioceptive stimulus opens a window by which we can use DNS to improve our body's control of posture and movement. DNS exercises enable us to provide a regular proprioceptive stimulus that will create change in the body.
And isn't that why patients seek out chiropractors in the first place? They are coming to us hoping we will make a change in their body that not only provides relief, but also results in lasting changes they can maintain.
For more reading:
https://gallagherperformance.com/do-you-really-need-more-mobility/
https://gallagherperformance.com/dns-solves-pain-improves-performance/
https://gallagherperformance.com/solving-pain-influence-czech-rehabilitation-techniques/
https://gallagherperformance.com/chiropractic-rehab-dns-treatment/
https://gallagherperformance.com/powerful-innovative-approach-improving-body-functions/
12 Week Distance Training Client Results
This training client sought out our services for three primary reasons:
1) Rehabilitate a chronic recurrent low back condition that has prevented him from training with any type of intensity or frequency for over two years AND get back to training while staying healthy in the process
2) Get stronger while packing on some quality size, and
3) Regain the feeling of athleticism from when he played college football.
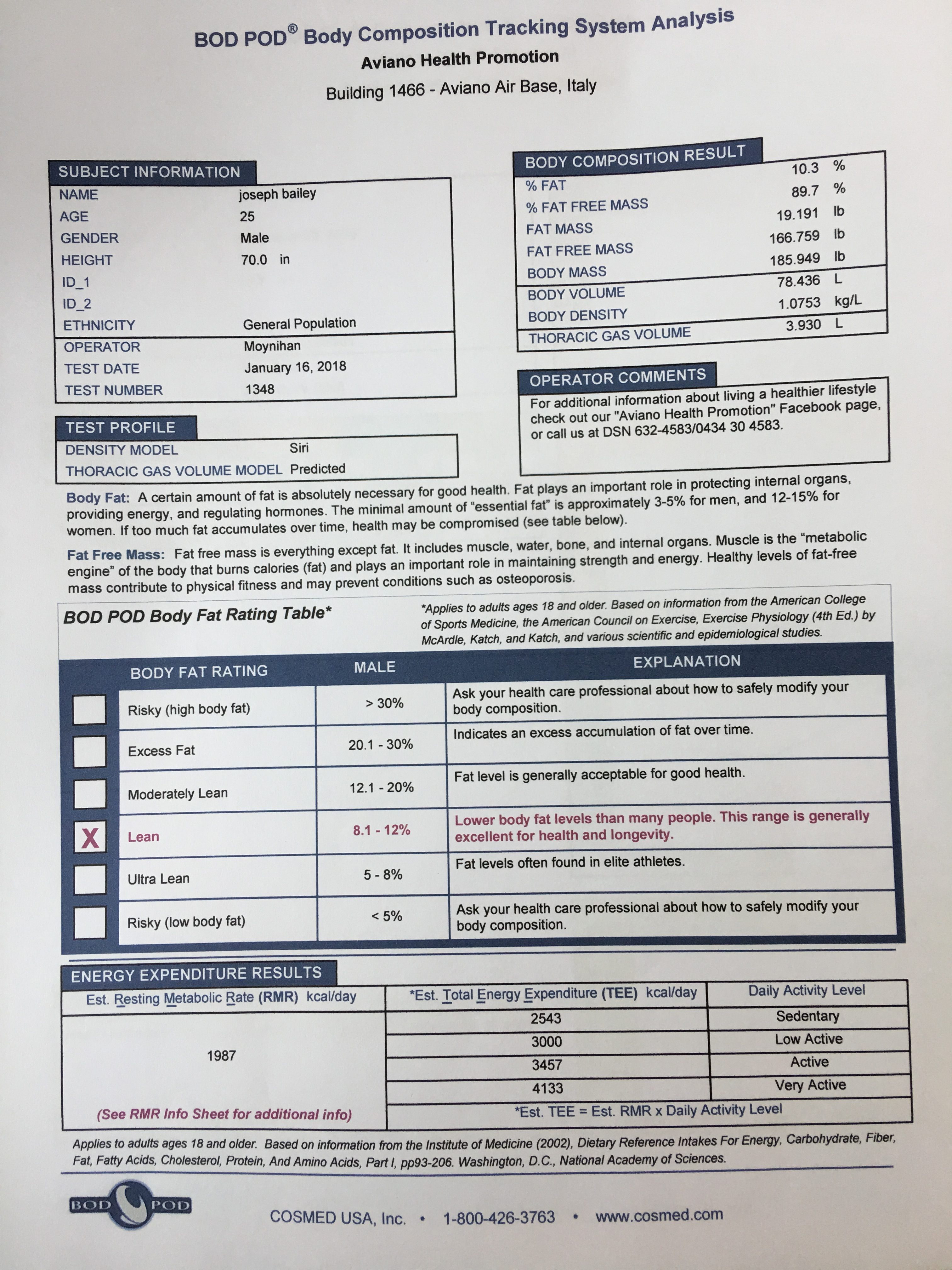
We recently concluded 12 weeks and during that time he had three BOD POD evaluations. Debate on the accuracy of the BOD POD aside, impressive changes were made in only 8 weeks. These evaluations occurred on 11/21/17, 12/19/17, and 01/16/18.
Some of the BOD POD highlights include:
- Fat Weight lose of 3.786lbs
- Body Fat % decrease from 12.6 to 10.3
- Fate Free Weight gain of 6.745lbs
- Body Weight increase from 182.9 to 185.9
Images 1-3. BOD POD results from 1/16/18. This was the third, and most recent, analysis during an 8-week period.
Included below are photos of a few of his training weeks to give you a glimpse of how his training was structured. Along with the changes seen in his body composition, his strength continues to progress and he is training with weights and a frequency that he has not seen in over two years while maintaining a healthy feeling body.
Exercise Hacks Ep. 6 - Deadlift Variations for a Functional Core
[embed]https://www.youtube.com/watch?v=W6qNeTnJdyU[/embed]
In this video we discuss two deadlift variations that will build rock solid functional core strength - the suitcase deadlift and pitchfork deadlift.
The suitcase deadlift and pitchfork deadlift are two deadlift variations that will expose energy leaks and strength imbalances real quick. Building a functional core often requires unconventional methods that go beyond aesthetically driven exercises. While unconventional these exercises force the lifter to generate total body tension to complete the lift - which makes them an awesome tool to teach lifters how to generate and maintain tension during squats, deadlifts or heavier training.
Each variation offers something unique.
1) The Suitcase Deadlift - targets the lateral stabilization system or lateral line in the body as detailed in Anatomy Trains. The lateral line will create or resist lateral bend in the body and serves as a 'brake' for lateral and rotational movements of the trunk. The lateral line runs in balance on both the right and left side of the body from the skull down to the trunk and lateral aspect of the hips, thighs, calves and mid-point of the foot.
2) The Pitchfork Deadlift - this variation of the pitchfork deadlift also targets the lateral stabilization system while forcing the lifter to resist rotation. It really hammers the spiral line detailed by Thomas Myers in Anatomy Trains. The spiral line is responsible creating or resisting rotations in the body. The spiral line is a myofascial sling that includes musculature that begins in the neck down to the opposite shoulder and then to the same side hip, knee, and foot arch, then up the back of the body to rejoin the fascia on the skull.
The bonus is both these exercises will reinforce patterns of stabilization in the body that are essential to movement.
These exercises are advanced and it is not recommended to go try them just to see if you can do them. They require a certain level of stability, coordination and strength to be able to do. Respect the process needed to progress to these exercises.
More related reading:
https://gallagherperformance.com/movement-improves-brain-function/
https://gallagherperformance.com/athletes-do-not-need-balance-to-be-successful/
https://gallagherperformance.com/the-essentials-of-speed-training/
https://gallagherperformance.com/fascia_muscular-adhesions_how_they_relate-_to_pain_and_overuse_injuries/
https://gallagherperformance.com/the-best-exercise/
The Beginner's Guide to Injury Recovery
Although we’ve worked with a broad spectrum of athletes - high school, collegiate, professional, former World’s Strongest Man, and elite triathletes - we work with just as many weekend warriors and those who simply love to be active. Whether it’s improving your running distance, increasing strength in the gym, or swinging a golf club without pain, we want to help you achieve your goals.
We also successfully treat those with overuse injuries, enabling them to return to the highly active lifestyle they enjoy.
Being active is an essential part to a healthy lifestyle. The many benefits of movement and exercise are well documented. Unfortunately, injury can become a reality for those that live an active lifestyle. When injury occurs, the effects are not only physical, but psychological as well. It is easy to become frustrated when your active lifestyle has been interrupted and concerned when you aren’t healing or turning around as quickly as you had hoped. Recovery from injury is a process that must be understood, appreciated and respected.
To help you better understand how to manage your own recovery from injury, here is a short list of items to be aware of so that you can respect the healing process and set yourself up for a timely and safe return to sport or activity.
Avoid Complete Rest
When injury occurs, it is often advocated to rest. Rest is a critical part of healing and the amount of rest one needs will be determined by the severity of the injury. Injury is a balance of load and capacity of tissues within the body. Once we exceed the capacity of a tissue (bone, ligament, muscle, tendon, disc, etc.) with a certain load, injury occurs. Rest helps restore the capacity of tissues by minimizing or removing load and thus allowing healing to occur.As critical as rest is to the healing process, movement is equally, if not more, critical. In the absence of severe injury and conditions where movement would be contraindicated (i.e. fracture, dislocation), movement serves to facilitate healing. The majority of musculoskeletal injuries heal best when we don’t avoid activity, but rather when we modify activity. The important factor here being that one finds activities they can perform without pain and that will facilitate healing through movement. This may be as simple as walking or gentle range of motion exercises. However knowing exactly what you should do for your specific injury can be a complicated answer. This brings me to my next point.
Don’t Rely on Social Media Gurus to Solve Your Injury
When injury occurs, people want a definitive answer when it comes to what they injured and how to manage it. And there are growing numbers that are seeking this information out online without ever consulting a licensed healthcare specialist. This could be due to frustrations with the medical model, a growing consciousness to seek out “non-traditional” or “alternative” therapies, or simply wanting to avoid paying out of pocket when there is free information available online. There can be the mentality of, “Why pay someone to fix me when I can learn to fix myself?” Not that this is wrong, but please understand that there are limitations when it comes to purely trying to self-manage your injury.Let me illustrate this point with an example of someone who may go onto an internet forum or social media page and state, “If have an L4-L5 disc bulge with sciatica, what exercises should I do to help me get out of pain?”
If you are seeking an answer out online, keep in mind the most appropriate answer you should receive is, “It depends”.
Any advice you receive from someone who hasn’t evaluated you is truly just throwing darts in the dark and hoping something sticks. Most people on the internet and social media who are offering up advice when it comes to injury rehabilitation are not licensed to do so, thus you should be skeptical. Many of these same people try to position themselves as an expert for one reason or another, but reality remains they are not a licensed professional and thus you should be skeptical. Skeptical because how can someone tell you what to do when they haven’t evaluated you – in person.
When it comes to injury rehabilitation, the evaluation process is the most critical step to ensure no time is wasted in the early phases of rehab and to minimize complications. Evaluations should consist of orthopedic and neurological testing as well as biomechanical/functional testing to evaluate for structural pathology, movement sensitivities and functional deficits.
The sharing of symptoms through some online medium is extremely limited in its value and it inherently creates bias. It will bias the feedback and direction you receive from who you are seeking advice from since all they have to operate off of is what you tell them. But when you are evaluated live, in person, by a licensed professional, bias can fall by the wayside when things are discovered that you may not feel are all that important or relevant to your present injury. Yes, history and understanding your problem is important, but it’s only a part of the puzzle.
This is because as professionals, we are trained to evaluate with our eyes and hands to assist in the diagnosis of your condition.
Seek Out Professional Evaluation and Treatment
There are numerous products and programs currently online that essentially attempt to remove the need for someone to see a licensed professional for an injury or ailment. These products or programs will draw people in as they hope to learn what they can do to fix themselves. There is nothing wrong with that, as self-management strategies are important for anyone to learn. People who are dealing with pain or injury must learn why their pain or injury developed in the first place and what they can do to help prevent it from returning.However the limitation to these products or programs is that they are mass marketed, attempting to appeal to a large audience and, therefore, are very general in nature. They are incapable of being highly specific to the individual. These programs or products may work for some, but when someone needs more individualized solutions they need to turn to a licensed professional such as a chiropractic rehabilitation specialist or physical therapist who approaches injuries and ailments from a functional perspective, not solely based on structural pathology.
Specialists exist for a reason. When your in-home or self-management strategies fail or if you are having persistent or worsening symptoms, you should seek out professional consultation. Specialist such as sports medicine physicians, rehabilitation chiropractors and physical therapists are capable of providing solutions to pain and injury through either diagnosing your condition, devising a rehab plan, and providing treatment. Massage therapists are another specialist to consider as many ailments and injuries have soft-tissue components that respond favorably to massage therapy by reducing pain and restoring muscle function.
Recognize the Gift of Injury
The recovery from injury is as much mental as it is physical. Believe it or not, there is a gift of injury – forced discipline.What do I mean by forced discipline?
Injury often times forces us to confront the very reasons why we got injured in the first place. The reason could be faulty mechanics, sharp increases in workout or training volume, or ignoring warning signs our brain was sending us.
Professional specialists mentioned above should assist in the process of helping you recognize the reason(s) for your injury and given you the direction needed in your recovery. But it's upon you to be disciplined and mindful during your recovery process and beyond. This new sense of discipline can apply to making better decisions when it comes to your rehab program, your posture, your movement, and the amount of stress or work you place upon your body.
Failure to do so can often lead to someone rushing his or her own recovery, returning too soon to sport or activity or frequent relapses. Be disciplined and regain control of your body.
Understand the Science of Pain
Failure to apply discipline in your recovery can also result in the feeling that your injury will never heal. The reality is all injuries heal. But long after the site of injury has healed, pain can still persist. Pain becomes a reminder to some that they aren’t healed. They will believe they are still injured.“So if my injury is healed, then why am I still in pain?”
Pain is a message from our brain that is meant to protect us. Even though pain is meant to protect us, pain is not a reliable source of indicating the extent of an injury or even where the injury is located. The classic example here is phantom limb pain. Amputees regularly will experience this phenomenon. One may experience left leg pain, yet they do not have a left leg. If pain is purely related to damage or injury, how would one experience pain in a limb that doesn’t exist?
The reality of pain perception can be a difficult education point as this is typically a new concept for the majority of patients and one they may need some time to understand. But it’s critical as their beliefs about pain can complicate the recovery process. It’s extremely beneficial for patients to learn about pain and address fear-avoidance behaviors and other factors that will interfere with reactivation into normal movement, activities of daily living and sport.
Gradual exposure to correct movement which takes stress of tissues can help to desensitize the brain to pain signals. Movement re-education serves to reduce pain signaling in the brain. As one learns to move better, pain goes down. You need to break your pain cycle with a better movement solution. It’s that simple.
Wrapping Up
Thanks for reading. We hope this post was helpful. Please leave any comments or questions you may have. Share this post with those who you feel can benefit from understanding how to better approach recovering from injury or pain.More related reading:
https://gallagherperformance.com/resetting-bodys-function-post-injury/
https://gallagherperformance.com/the-hidden-causes-of-sports-injury/
https://gallagherperformance.com/technique_and_performance/
https://gallagherperformance.com/nutrition-for-faster-recovery-from-injury/
https://gallagherperformance.com/improved-approach-chronic-pain-management/
https://gallagherperformance.com/effective-treatment-shoulder-pain/
Clinically Pressed Podcast Episode 38
[embed]https://www.youtube.com/watch?v=3oAEjdiQK1A&feature=youtu.be[/embed]
Clinically Pressed Podcast Episode 38
Had the opportunity to sit down with Joel and Kyle of Clinically Pressed and answer their questions.
Clinically Pressed is committed to sharing as much useful and applicable information as possible to their audience. Comprised of a PhD, DC and ATC, the CP podcast that seeks to make the complicated simple. CP wants to connect you with experts in their fields - all at no cost to you. They want their audience to be able to access information as easy as possible. Be sure to check them out on the web, on their social media, and support them on Patreon. Also be sure to check out their free weekly newsletter - Total Athletic Therapy.
Website: clinicallypressed.com
Facebook: Clinically Pressed
Instragram: Clinically Pressed
YouTube: Clinically Pressed
Newsletter: Total Athletic Therapy
From the Clinically Pressed website, here the notes from the show:
0:00- Episode introduction and check out Paragon Nutrition for some of the most effective and well done supplements on the market. Use code “CP15” for 15% off at check out.
1:26-CP Intro Video: Courtesy of Justin Joy of “Elder Pine Media” Contact:
2:04-Welcome Sean Gallagher DC of Gallagher Performance and the connection to Palmer College.
3:38-The sports injury department at Palmer and it being one of the only in the country.
6:00-Dr. Juehring of Palmer and his clinical experience along with his athletic background make him one of the hidden gems in the industry.
What Makes a Sports Rehabilitation Chiropractor?
Chiropractors have traditionally been known for treating patients suffering from acute or chronic pain related to the neck and back. Chiropractic treatment that involves spinal manipulation is regarded as a standard for treatment of cervical spine (neck) pain and acute lower back pain. Not only is it safe, but it has also shown tremendous health benefits for improving range of motion and reducing pain in patients during the rehabilitation process.
However, chiropractors are also capable of helping patients rehab and recover from injuries suffered in an accident or sports. The role chiropractors play in rehabilitation and sports medicine has grown substantially in the last 10 years. Almost all professional sports teams in North America utilize chiropractic services because of the recognition chiropractors has received in their ability to help athletes perform at their highest possible level. Apart from this, many rehabilitation clinics include chiropractic care as part of the services offered to patients.
Consider for a moment that the Managing Director for Sports Medicine for the United States Olympic Committee is Dr. Bill Moreau....a chiropractor!
Holding a position as a sports rehabilitation chiropractor is growing in popularity and, just like an athlete, a sports rehabilitation chiropractor must possess many tools or skills to be both effective and efficient in treating patients who are active and athletic.
Below is a list out 5 critical elements you should find when looking for a chiropractor who will be capable of treating you from a rehabilitation or sports injury perspective. Consider that these are not simply just my opinion, but rather this list has been compiled based on the insight of several of my colleagues and mentors, their clinical experience, as well as my own clinical experience.
- Palpation & Adjusting Skills. The heart of chiropractic is the ability to assess, diagnose and treat (heal) with our hands. Our hands truly are the greatest diagnostic tool available to us. I've had people say to me that what I do as a chiropractor is "easy" and that "anyone can adjust". There is some truth to that. Adjusting is easy. You can make a joint "pop" real easy. The challenging part is palpation and finding exactly what joint needs corrected, what motions are limited, and determine exactly how you will adjust the dysfunctional joint(s). Palpation is a skill and takes years to refine. You would be wise to find a sports rehabilitation chiropractor who is very skilled with their hands and capable of determining appropriate application of chiropractic adjustments.
- Functional Approach to Evaluation and Treatment. The use of functional evaluations is another critical skill of the sports rehabilitation chiropractor. The ability to assess movement and identify hidden causes to injury and pain become invaluable to helping patients find relief and optimize performance. If your chiropractor isn't taking time to assess your movement and helping identify how it may be playing a role in your pain or injury, you may be miss reasons why your pain is recurrent or why you just can't seem to get better.
- Functional Rehabilitation. A sports rehabilitation chiropractor should incorporate rehabilitation and active care into your treatment plan. Almost every case involving muscle or joint pain requires some level of strengthening exercise progression and education. The functional approach to rehabilitation includes identifying joint dysfunction, muscular imbalances, trigger points, and faulty movement patterns. These are often the hidden causes of injury. Observing how a patient moves and functions allows us to identify improper movement patterns that become contributors to pain and poor sport performance. By placing an emphasis on strategies to improve movement and function, functional rehabilitation is effective in improving qualities of endurance, strength, stability, balance, agility, coordination, and body awareness.
- Dynamic Neuromuscular Stabilization (DNS) and Vojta Therapy. DNS and Vojta Therapy are advanced approaches used to not only treat a variety of neuromuscular conditions but also used by athletes worldwide to elevate performance. By applying principles and techniques rooted in the study of child development, DNS and Vojta Therapy aim to improve and restore the activation ideal movement patterns. These techniques are used to promote the ideal postures, movements, and degree of body awareness that is essential not only to athleticism, but to also treating the underlying causes of several pain syndromes that are commonly treated by sports rehabilitation chiropractors.
- Myofascial Release & Manual Therapy Techniques. Myofascial release targets adhesions that develop either within a single muscle or between adjacent muscles and other forms of connective tissue such as fascia, tendons and ligaments. Sports rehabilitation chiropractors commonly use myofascial release & manual therapy techniques such as cross friction massage, active release, instrument assisted soft tissue mobilization, muscle activation, PIR, and PNF. Many athletes and patients experience accumulative or overuse trauma (ex: plantar fasciitis due to running or carpal tunnel syndrome due to prolonged computer/desk work). The goal becomes to work a muscle to remove adhesions and restore neuromuscular function to decrease pain while increasing range of motion, strength, and coordination of movement.
More related reading:
https://gallagherperformance.com/prevent-re-injury-integrated-training-rehabilitation/
https://gallagherperformance.com/before-you-go-to-a-chiropractor-read-this-first/
https://gallagherperformance.com/fascia_muscular-adhesions_how_they_relate-_to_pain_and_overuse_injuries/
Scoliosis Treatment for Children & Teenagers
Scoliosis.
The diagnosis can make anyone uneasy and it can become even more unnerving for parents when they hear that diagnosis for a child. Scoliosis in children between the ages of 10-18 years of age is termed adolescent scoliosis and can be due to many causes. But the most common type of scoliosis in the adolescent period is one in which the cause is unknown and is called adolescent idiopathic scoliosis (AIS). The reason why it is called idiopathic scoliosis is because there are currently no identifiable reasons as to why scoliosis develops in these children.
When we consider the current limited understanding of scoliosis in a traditional medical sense and the limitations in medically accepted treatment of AIS, it makes one wonder if there is a model of evaluation, treatment and management of scoliosis that may provide the potential for deeper understanding of the condition and reasons why it develops. Possibly bringing to light conservative treatment measures that have the ability to stop it's progression - or even reverse it.
Before we get to more detail on these discussion points, lets review what is currently known about AIS, from symptoms to treatment.
Symptoms
AIS generally does not result in pain or neurologic symptoms in children and teenagers. I can't stress this enough as often times this is the reason why the diagnosis of scoliosis can blindside many. Again, your child or teenager often times has no pain and no complaints. They seem to be perfectly healthy, active kids. This is a big reason why often times, scoliosis is either identified by primary care physicians during routine annual exams or during school exams.
While there may be no pain present and the child seems to be otherwise healthy despite curvature changes in the spine, how serious can the condition really be if it isn't that limiting?
While pain and neurologic symptoms may not be present, there can be disturbances within the nervous system on the cerebellar and sensory-motor integration level (1). Often there can be altered reflexes as identified by Janda, hypermobility, and muscular imbalances which create functional changes within the body (1). These functional changes have a direct effect on movement, thus having a direct effect on structure. In this case, the curvature of our spine (structure) is directly related to the function of our musculature and movement system.
Disturbances within our muscular/movement system can be identified by functional evaluation, however these evaluations are not typically part of the traditional medical evaluation process.
Does this lack of functional evaluation potentially leave pieces of the scoliosis puzzle unsolved? Pieces that would aid in determining the most appropriate course of treatment and management - and potentially a patient-specific reason for the development of the condition?
Evaluation & Physical Exam Findings
Classically, the physical evaluation and physical exam of a child diagnosed with AIS has a few key findings:
- Visible signs of lateral spine curvature along with asymmetries seen in the shoulders or hips, in which one side appears higher than the other.
- Adam's Forward Bending Test revealing either structural or nonstructural (aka functional) scoliosis. Adam's Test is consider the most sensitive test for scoliosis and the most common test used in the diagnosis of scoliosis.
- Radiographs or x-ray indicating positive findings for scoliosis. The curves are often measured for angles of the curves to determine severity.
Some functional evaluation considerations that are made from the world of Dynamic Neuromuscular Stabilization (DNS) include:
- Functional tests to assess movement control and coordination of the musculature surrounding the shoulders, spine, and hips.
- The central role proper neuromuscular function plays in spinal stabilization and optimal spinal posture.
- Sensory-motor integration and cerebellar function in the patient's ability to sense their body awareness, posture, and joint position in space.
- Hypermobility and other present musculoskeletal compensations in response to poor function of the integrated stability stabilization system (ISSS).
Treatment
Traditional medical treatment of AIS falls into three main categories:
- Observation
- Bracing
- Surgery
But are there other treatment options? Ones that may be considered more "alternative" yet may possess the potential to yield positive results in the treatment and management of children and teens with AIS?
Often interventions such as chiropractic, physical therapy, rehabilitation, and exercise therapy can be considered by some as alternative treatments to prevent progression of AIS. However, when applied appropriately in the treatment of AIS, these "alternative" treatments can offer something that observation, bracing, or surgery cannot - truly addressing the underlying functional causes in the development of structural asymmetries.
Improving the way one moves and functions - through targeted therapeutic exercise, joint mobilizations, and/or spinal manipulation - can have huge impact on preventing the progression of AIS. Coming from the Prague School of Rehabilitation, the pioneers of DNS therapy, they not only have success in treating AIS, they even have cases of reversal. Clearly there is something we can learn from the model utilized by DNS practicioners in improving our model of scoliosis evaluation, treatment, and management.
The hope is that this article has brought to light some reasons why we should reconsider how scoliosis is evaluated and treated as well as treatment options that exist, but can be rather difficult to find.
References:
- Cerebellar function and hypermobility in patients with idiopathic scoliosis, Kobesova A, Drdakova L, Andel R, Kolar P. International Musculoskeletal Medicine. , 2013, 35(3): 99-105.
For further reading on DNS and the importance of functional evaluation, please check out the links below:
https://gallagherperformance.com/dynamic-neuromuscular-stabilization-advancing-therapy-performance/
https://gallagherperformance.com/solving-pain-influence-czech-rehabilitation-techniques/
https://gallagherperformance.com/resetting-bodys-function-post-injury/
https://gallagherperformance.com/the-importance-of-functional-evaluation/
https://gallagherperformance.com/chiropractic-rehab-dns-treatment/
When Should I See A Chiropractor?
[embed]https://www.youtube.com/watch?v=1aaE3CIouTU[/embed]
In this video we discuss some important points to consider when to see chiropractor or why to see a chiropractor, especially one that has a sports injury and rehab specialization and practices in a functional movement model.
Some points to consider:
- How important is your health to you? Health is an investment and requires a proactive approach rather than be reactive.
- Do you want to get out in front of rather muscle tightness and joint range of motion/mobility restrictions before they get more serious or painful?
- Most people are unsure of who to see for back pain and joint pain, even muscle tightness. They may see their PCP, but not receive the answers or solutions they were hoping for. They are looking for a provider they can trust.
- Those that have a positive experience with a chiropractor or have one they trust, turn to them when they start to "feel off" or they feel their body is moving as it normally does or they start to feel pain.
- Ideally, chiropractors who have a specialization in functional rehab, sports injury, and movement are the experts you should see for the most musculoskeletal conditions that we commonly deal with.
- When, or if, you see a chiropractor is ultimately your choice and one that can prove to be beneficial and a worth while investment.
More related reading:
https://gallagherperformance.com/the-importance-of-functional-evaluation/
https://gallagherperformance.com/low_back_pain_treatments_that_just_wont_help/
https://gallagherperformance.com/solving-pain-influence-czech-rehabilitation-techniques/
https://gallagherperformance.com/powerful-innovative-approach-improving-body-functions/
https://gallagherperformance.com/effective-treatment-shoulder-pain/
https://gallagherperformance.com/solving-movement-problems-entertainment-vs-effective/
Chiropractic, Rehab & DNS Treatment
https://www.youtube.com/watch?v=ceIcoreYu8o&t=4s
This video illustrates how we integrate chiropractic, rehabilitation and dynamic neuromuscular stabilization (DNS) into patient treatment. For the purposes of this video, these techniques were used to speed up post-workout recovery, ensure structural balance and improve how the body functions. Similar to fine-tuning a race car, the human body can benefit tremendously from fine-tuning to keep body prepared for high performance.
Key take home points:
- Treatment is directed at patient-specific goals and outcomes. There are different levels of care that may need, ranging from symptomatic (i.e. painful conditions) to more performance-based therapy or fine-tuning.
- Chiropractic manipulative therapy (i.e. adjusting) was not filmed but utilized for the spine and hips.
- Soft-tissue work was done manually and instrument-assisted to mobilize muscle and connective tissue to improve recovery.
- Dynamic neuromuscular stabilization (DNS) was used to fine-tune motor patterns and muscular activation. Proper muscular activation and stabilization function of muscles helps to ensure proper muscular coordination while minimizing stress on the joints.
- This all adds up to optimizing performance while keeping the body as healthy as possible.
https://gallagherperformance.com/fascia_muscular-adhesions_how_they_relate-_to_pain_and_overuse_injuries/
https://gallagherperformance.com/dynamic-neuromuscular-stabilization-advancing-therapy-performance/
https://gallagherperformance.com/powerful-innovative-approach-improving-body-functions/
https://gallagherperformance.com/solving-pain-influence-czech-rehabilitation-techniques/
Resetting the Body's Function Post-Injury
"After an injury tissues heal, but muscles learn. They readily develop habits of guarding that outlast the injury" - Janet Travell, MDGuarding after an injury is normal and it is to be expected. However, when left unidentified and untreated, guarding or protective patterns can become common reasons for chronicity and why someone "hasn't got better". This is why we must go beyond structural injury and think function in treatment rehabilitation.
From the functional viewpoint, we must evaluate for these guarding patterns that patients readily default to due to injury/pain. Identifying and treating these guarding patterns appropriately will often times enable patients to feel better almost immediately.
While yes it is important to evaluate for structural injury (fracture, dislocation, ligament sprains, tendinopathies, disc herniations, etc.) and manage them accordingly, the reality is these tissues will heal in time. However, after these injuries heal, there can be presentations within the body that create complications in achieving full recovery or become reasons for relapse.
Often times patients will complain about tight calves and hamstrings after spraining an ankle or tightness in their low back and hips after a disc rupture. Or they may have developed pain and/or sensitivities in other areas of their body seemingly unrelated to their initial site of injury.
The ankle ligaments will heal. The disc will heal. But the body will guard and protect and this becomes programmed within the nervous system. This is exactly what we need to treat for patients to get better and this new reality becomes very liberating for patients.
When patients come to understand that their injury has healed, but it's their brain and muscles that must re-learn how to work as they did before the injury, they become less fearful and more confident in a positive outcome. Essentially, they come to understand that we must reset their body so their neuromuscular function returns to pre-injury status.
To reset the right things in the body, we must assess and analyze the problem then utilize corrective measures in treatment and/or training. This system helps us develop efficiency in treatment and enables us to expect results.
What type of corrective measures? The gold standard becomes manual therapy and therapeutic exercise. When combined, these serve to get patients out of pain and improve the function in their body.
Yes these results can often times be rather immediate, however in some cases recovery can test a patient's patience as the process may be slower than they aniticipated.
When progress is slow, it is important to remember the following:
- Therapeutic exercise is the most evidence-based treatment.
- Passive treatments (tape, modalities,etc.) may offer temporary relief but are not helpful in medium and long term recovery.
- Injections and surgery have been not shown any greater effectiveness in outcomes than exercise.
- Seek advice and treatment from a licensed professional who specializes in functional movement. Ideally this would be a rehabilitation chiropractor or physical therapist with movement specializations are the gold standard here. These practitioners focus on the functional paradigm of manual/physical medicine. And no, your "functional trainer" at the gym doesn't count.
- Self-management is key. Reduce activities that provoke pain, apply gradual exposure to activities to build confidence and tissue capacity through exercise. Exercise must be tailored to you to reduce pain and improve strength and function throughout your entire body.
- Progress load and exposure gradually. The key is to be consistent with your exercise therapy. Forget about how much you were doing before the injury and what others are able to do. Everyone responds differently. Focus on your recovery and what works to get you back on track.
- Getting back on track can take a long time. In some cases, upwards of 3 to 12 months depending on a number of factors including duration of symptoms, functional deficits and patient compliance during their exercise program. Keep in mind, other treatments can offer faster recovery but nothing has demonstrated better long-term results than progressive exercise.
More related reading:
https://gallagherperformance.com/the-importance-of-functional-evaluation/